A positive patient experience results from thoughtful, attentive, and empathetic care, which impacts adherence to the treatment plan and the patient’s healing process.
A fulfilling relationship between a patient, their family, and their care team builds the patient’s trust in the practice/department and enhances the patient experience and the reputation of the practice/department.
This page provides tools, resources, and NRC Health patient survey information designed to address patient expectations and optimize their experiences.
Whether we provide patient care directly or indirectly, we are all responsible for fostering a welcoming environment for our patients, their families, visitors, and our colleagues. Mass General uses a four-part model called “icare” to help us live by the words of our mission and credo. The icare model provides a set of simple reminders that every one of us, regardless of role, impacts the patient experience.
See below for details of the four icare standards – Communicate, Advocate, Respect, and Empathize – and comments describing each through the voice of the patient. These patient verbatim comments demonstrate the importance of utilizing icare consistently during every patient, family member, visitor, and colleague interaction and highlight best practices as well as areas of opportunity to improve. Using the icare model benefits everyone (patients, families, visitors, and fellow employees), as it:
- Supports the Mass General Mission
- Is the right thing to do
- Helps patients feel welcomed and supported, which is frequently mentioned in patient survey verbatim comments
Description | Example Comments |
I communicate in a warm and welcoming manner.
|
|
I advocate on behalf of patients, families, colleagues, and myself.
|
|
I respect and embrace differing values, opinions, and viewpoints.
|
|
I empathize and acknowledge the feelings of others.
|
|
To help staff understand and implement icare:
- Ensure all staff view the icare video.
- Complete a customized icare Learning Lab Session.
- Learning Lab session content consists of core icare content and customized content specific to your practice/department/service area.
- Customized content is created for each individual practice/department/clinical service area and role group based on:
- Pre-icare rollout discussion and, if applicable, observations
- Patient Experience survey results
- Other areas of focus as requested by Practice Managers (if needed)
- To schedule an icare Learning Lab in your area, please contact MGHpatientexperience@mgh.harvard.edu.
- Reinforce icare standards regularly and recognize/reward staff for exemplifying icare standards. This includes:
- Reviewing bi-weekly icare Huddle Messages with staff
- Speaking to icare standards during every staff meeting
- Identifying staff challenges that may hinder staff from consistently utilizing the icare model
- Recognizing and/or rewarding staff members who personify the elements of icare with their patients, family members, visitors, or colleagues
- Sharing patient feedback, letters, and/or Patient Experience survey verbatim comments
- Linking the icare standards to patient survey comments
Please contact us at MGHpatientexperience@mgh.harvard.edu if you wish to be added to our bi-weekly icare Huddle Message distribution list.
To learn more about icare and additional resources available (including a repository of all past icare Huddle Messages), please visit the Patient Experience page on Apollo.
Telephone calls are often the first point of a patient’s contact with a practice. First impressions are formed within one-tenth of a second and may set the tone for the entire conversation, so it is important to portray the practice positively from the start.
- Use the four-part greeting:
- Greet the caller.
- Introduce yourself.
- Introduce your department.
- Ask how you can help.
- Follow the hold and transfer protocols: always ask the caller for permission.
- Use a warm, friendly tone of voice and smile: patients can “hear” your smile.
- Listen attentively.
- Use the two-part closing:
- Before ending the call, ask, “Is there anything else I can do for you?”
- End the call with “Thank you.”
- Use a standard voicemail greeting.
- Use a standard out-of-office message.
For additional resources and recordings of previously held trainings on this topic, click here.
For more information on phone management, click here.
Patients need and expect to be welcomed and acknowledged at check-in.
- Greet patients with a warm smile and a pleasant tone of voice, and thank them for coming.
- Establish eye contact.
- If you’re busy with another patient or taking a call, acknowledge that you are unable to greet the patient promptly and tell them you will be with them shortly, being mindful of your facial expression, tone of voice, and body language.
- Understand and use protocols to accommodate patients who are late for appointments.
- If a patient arrives up to 20 minutes late, try to accommodate them within the appointed session. If necessary, offer the end-of-clinic slot.
- If a patient arrives more than 20 minutes late, try to accommodate them; if you cannot, offer the option to reschedule or to see another clinician.
- If the patient is upset, use the LEAD model (Listen, Empathize, Apologize, Do the Right Thing) to provide service recovery. Offer the opportunity to reschedule or see another clinician, if appropriate and if a time slot is available.
- Notify patients if the schedule is running late, estimate how long the wait might be, and apologize.
- Regularly inform patients in the waiting room of wait times.
For additional resources and recordings of previously held trainings on this topic, click here.
Patients want to be informed of any delays at check-in. Offering an estimated wait time and a sincere apology for any inconvenience will help to set a positive tone for their visit.
- Apologize for delays and longer-than-anticipated wait times.
- Offer comfort items when possible (e.g., magazines).
- Make announcements in the waiting room when wait-time boards are updated.
- After each update, let patients and families know when they can expect another update.
- If the appointment is 15 minutes or less late:
- Apologize for the delay on behalf of the practice.
- If appropriate, let the patient know that the clinician is tending to a patient issue (in accordance with HIPAA, do not provide any specifics about the issue).
- If the clinician is running more than 15 minutes late (or another duration as identified by your practice/department):
- Notify the patient that the clinician is behind schedule and let them know when you will update them next.
- Offer to reschedule the appointment.
- Notify the practice manager that the clinician is running more than 15 minutes late.
- The practice manager should notify clinicians that they are 15 minutes or more behind schedule and ask them to apologize to all patients upon greeting them and to thank them for waiting.
For additional resources and recordings of previously held trainings on this topic, click here.
Service breakdowns refer to any interruption to the planned or expected operational aspects of care. Unexpected events will inevitably occur and how we respond influences the patient’s perception and overall experience. Each situation is different and will require good judgment for effective handling. When a service breakdown occurs, patients and families want their concerns to be acknowledged and resolved (or to be offered options for resolution).
- Use the LEAD model when addressing patient complaints:
- Listen: Allow the patient/family to feel heard (“I hear you saying…,” “I understand you’re frustrated…”).
- Empathize: Notice and acknowledge feelings (“I can understand why you are upset…”).
- Apologize: Acknowledge error without placing blame on anyone, and apologize on behalf of the hospital for the inconvenience (“I apologize for the wait.” “I apologize for the inconvenience.” “I will keep you informed.” “Is there anything I can do to make you more comfortable during your wait?”).
- Do the Right Thing: Determine the best, most timely solution.
- Escalate issues promptly to a manager when the situation cannot be immediately rectified.
For additional resources and recordings of previously held trainings on this topic, click here.
Patients want to be acknowledged at checkout and, if necessary, helped with future appointments, lab work, referrals, questions, or other needs. Patient checkout is the last opportunity for patients to have a face-to-face interaction with staff, so it is important to ensure they are fully satisfied with this exchange.
- Acknowledge patients and ask how you can help them.
- Ask patients if they have any questions.
- Thank patients for coming to Mass General.
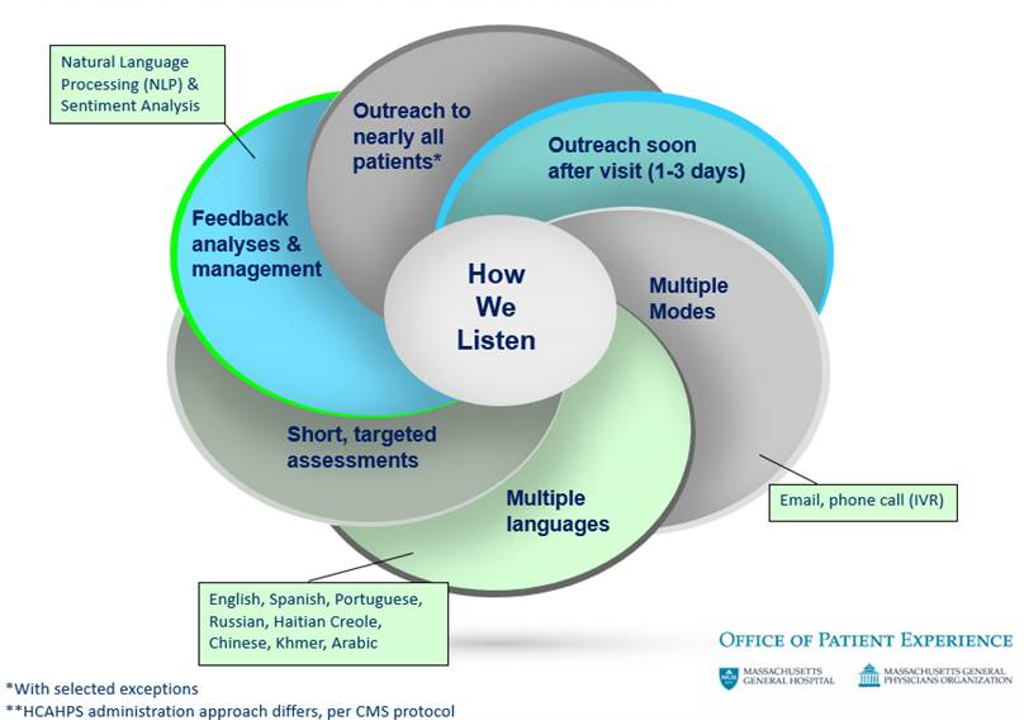
Mass General partners with NRC Health to collect feedback on an ongoing basis from patients about their care experiences. This partnership enhances our efforts to understand and improve the patient experience. NRC Health serves as the single patient experience vendor across Mass General Brigham.
Results and comments are distributed to practice leadership regularly to guide improvement efforts.
The image below is a high-level overview of how our NRC Health patient outreach works and what it entails:
To help staff understand what patients are being asked and how the practice/department is doing:
- Review and share weekly/monthly verbatim comments.
- Review and share NRC Health results (e.g., data, comments) at staff meetings.
- Post results in a visible location for staff such as in a staff lounge or meeting room.
- Identify trends and opportunities for improvement and identify best practices for those metrics that are above average.
- Develop an annual improvement plan.
To learn more about our NRC Health outreach to patients, including benefits of this feedback, and frequently asked questions, click here.
- Office of Patient Experience on Apollo
- icare Model
- MGHpatientexperience@mgh.harvard.edu – email the Office of Patient Experience to
- receive the biweekly icare Huddle Messages via email
- request a customized icare Learning Lab session for your practice/department/clinical service area
- obtain an icare poster for your practice/department/clinical service area
- obtain a supply of icare badge tags for you and/or your staff





